Immune tolerance: a scientific explainer on this biological process
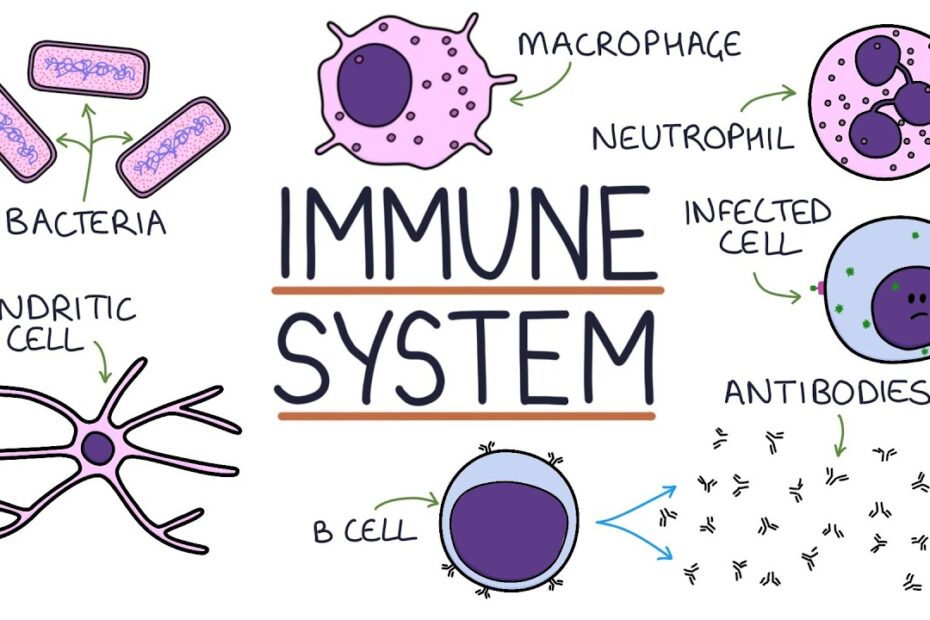
Immune tolerance is a critical biological mechanism that prevents the immune system from attacking the body’s own tissues, a process known as autoimmunity. First described in the 1940s by Sir Frank Macfarlane Burnet and Peter Medawar, the concept of immune tolerance was further elucidated through their work on the “self-nonself” model. This process involves the deletion or inactivation of self-reactive lymphocytes during their development in the thymus (for T cells) and bone marrow (for B cells), a phenomenon termed central tolerance. Peripheral tolerance mechanisms, such as regulatory T cells (Tregs) and anergy, further ensure that any self-reactive lymphocytes escaping central tolerance do not cause harm. Dysregulation of these processes can lead to autoimmune diseases like rheumatoid arthritis, type 1 diabetes, and multiple sclerosis, as highlighted by research from institutions such as the National Institutes of Health (NIH) and the European Federation of Immunological Societies (EFIS).
Recent advancements in immunology have revealed the role of specific molecules and pathways in immune tolerance. For instance, the CTLA-4 and PD-1 pathways are crucial for maintaining peripheral tolerance by suppressing T cell activation. The discovery of these pathways, which earned James P. Allison and Tasuku Honjo the 2018 Nobel Prize in Physiology or Medicine, has revolutionized cancer immunotherapy. Additionally, studies published in journals like Nature Immunology and Science have identified microRNAs and epigenetic modifications as key regulators of immune tolerance. Organizations such as the Immune Tolerance Network (ITN) continue to investigate therapeutic strategies, including tolerogenic vaccines and stem cell therapies, to modulate immune responses in autoimmune diseases and transplantation.
Key Mechanisms and Implications of Immune Tolerance
- What is central tolerance? Central tolerance occurs during lymphocyte development in the thymus and bone marrow, where self-reactive T and B cells are eliminated or inactivated to prevent autoimmunity.
- How do regulatory T cells contribute to immune tolerance? Regulatory T cells (Tregs) suppress the activation of self-reactive lymphocytes in peripheral tissues, maintaining immune homeostasis and preventing autoimmune responses.
- What are the clinical applications of immune tolerance research? Research on immune tolerance has led to therapies for autoimmune diseases, organ transplantation, and cancer, including immune checkpoint inhibitors and tolerogenic vaccines.